Study objectives: We created in situ femoral vein thrombi in swine to investigate the response of the latex d-dimer signal to acute in situ venous thrombosis, and to determine the minimum dose of exogenous bolus tissue plasminogen activator (t-PA) required to significantly elevate the d-dimer signal.
Study design: We studied seven swine (20 to 22 kg) under pentobarbital anesthesia. A 6-cm segment of the proximal femoral vein was surgically exposed and briefly ligated. Thrombin, 250 U, was then injected into the isolated femoral vein segment to create an in situ clot. After clot formation was documented to be complete between the ligatures, they were then released. D-dimer levels were then measured every 15 min for 1 h before and 1 h after clot formation with ligatures released. Time-response curves to establish timing of peak t-PA effect were performed, and then escalating dose-response curves of d-dimer level to minidose t-PA were plotted.
Results: After formation of the clot, the release of ligatures resulted in no change in d-dimer levels over 1 h (p = 0.62) in all swine. When a time-response curve to exogenous t-PA bolus in the presence of femoral clot was plotted, there was a maximal increase in d-dimer signal at 30 min after bolus t-PA administration. The subsequent dose-response curves for escalating fivefold boluses of minidose t-PA showed an increase in d-dimer signal at doses of 0.8 mg (p = 0.03) and 4 mg (p = 0.003).
Conclusion: We conclude the following: (1) in situ femoral vein clot formation does not elevate d-dimer signal for 1 h after ligature release; (2) minidose t-PA boluses of 0.8 mg and 4 mg significantly elevated the latex d-dimer signal above baseline; and (3) there is a potential role of minidose t-PA in enhancing the d-dimer signal in in situ deep venous thrombosis.
Key words: in situ clot; latex d-dimer signal; minidose tissue plasminogen activator
Abbreviations: ELISA = enzyme-linked immunosorbent assay: t-PA = tissue plasminogen activator
**********
Venous thromboembolism is manifested by deep vein thrombosis and pulmonary embolism. It is a significant cause of mortality and morbidity, especially in hospitalized patients. There are 250,000 hospitalizations and 200,000 deaths per year in the United States secondary to pulmonary embolism, of which deep vein thrombosis is the primary cause. (1) It is also known that approximately 10% of in-hospital deaths are secondary to venous thromboembolism, which are potentially preventable. (2) Clinical evaluation frequently fails to identify the diagnosis antemortem, and postmortem studies of venous thromboembolism have routinely found that the majority of cases with fatal severe thromboembolism have not been diagnosed antemortem. (2) It is in this setting that many efforts have been directed at developing a more effective algorithm for promptly diagnosing thromboembolic disease and allowing treatment to be efficiently prescribed. One such attempt is the plasma d-dimer assay, which constitutes an antigen-antibody reaction to the dimeric final degradation product of a mature clot. (3-6) These tests have been classified as latex and enzyme-linked immunosorbent assay (ELISA). The latex test has the advantage of rapid availability and is applicable to single samples in individuals. (6) The ELISA test generally requires batching of samples. (6) Several studies have shown a high sensitivity for pulmonary embolism using the latex d-dimer test. (6,7) The sensitivity of this test for lower-limb deep vein thrombosis is less than that for pulmonary embolism, with sensitivities of 83% and 92%, respectively. (7) This is obviously inadequate for use as a single screening tool in the evaluation of patients suspected of having deep vein thrombosis. Another problem of the latex test is its low specificity, approximately 68% for deep vein thrombosis and 54% for pulmonary embolism. (7)
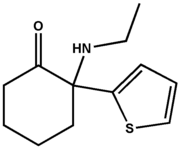
We hypothesized that mechanical breakdown of a clot in the central circulation allows easier access of endogenous thrombolysis to the clot migrating from the legs. We postulated that an in situ clot formed in the legs, blocking off a venous channel completely, would not allow enough contact between the clot and the circulation to mount significant endogenous thrombolysis. We hence developed a protocol to assess the dose-response relationship between exogenous minidose t-PA (Activase; Genentech; South San Fransisco, CA) and the latex d-dimer signal (IL-Test D-dimer; Instrumentation Laboratory; Lexington, MA) in in situ lower-limb thrombus. There is a suggestion in the literature (8,9) that deep vein thrombosis can occur without elevation of d-dimer levels, and this may be due to low endogenous t-PA activity in the deep leg veins of elderly and asymptomatic patients. With insufficient clot dissolution, there is an inability to elevate plasma d-dimer signal above background noise. (8,9)
HYPOTHESIS
A peripheral "sequestered" clot in the lower limbs has a very low endogenous thrombolysis rate, resulting in the inability to elevate d-dimer levels above the normal reference range. These levels can subsequently be amplified by exogenous t-PA bolus injections.
PURPOSE
The purpose of the study was twofold, as follows: (1) to measure d-dimer levels over time after creation of an in situ femoral vein clot, to assess whether or not increases in d-dimer signal will occur after formation of the clot in swine; and (2) to determine the dose-response relationship to a minidose, exogenous t-PA bolus on d-dimer levels after acute, in situ femoral vein clot formation in swine.
MATERIALS AND METHODS
Seven swine weighing 20 to 22 kg each were sedated IM with a combination of tiletamine hydrochloride and zolazepam, 6.25 mg/kg, and xylazine, 4.5 mg/kg. Once sedated, an ear lobe marginal vein was cannulated for induction of anesthesia. Anesthesia was maintained with pentobarbital sodium, 25 mg/kg. Negative eye-blink reflex served as a marker of adequate anesthesia. Once this was achieved, intubation and mechanical ventilation under continuous pulse oximetry and ECG monitoring followed. Two initial blood samples for baseline plasma d-dimer levels were obtained 15 min apart before instrumentation of the swine. Next, an indwelling central venous catheter was placed in the right internal jugular vein and two more postinstrumentation blood samples were obtained 15 min apart. This line was used for subsequent blood sampling and administration of t-PA boluses. After central cannulation was achieved, dissection of the femoral vein was performed, involving meticulous ligation of posterior penetrating branches draining into the main femoral vein. A 6-cm length of vein was exposed and isolated, and ligatures were placed at the proximal and distal ends of the segment of exposed vein (Fig 1).
[FIGURE 1 OMITTED]
Local thrombosis was then induced by injection of approximately 250 U thrombin using a 25-gauge needle. In < 5 min, the presence of a clot was confirmed by development of a rubbery consistency to gentle palpation of the entire segment of vein between the tightened ligatures. At this point, both the proximal and distal ligatures were released, and serial d-dimer measurements (Fig 2, 3) were performed.
[FIGURES 2-3 OMITTED]
D-direct Sampling
We obtained four preclot samples, four postclot samples to asses clot stability without t-PA, and four to eight samples were obtained after t-PA administration. The initial four preclot d-dimer samples included two preinstrumentation and two postinstrumentation samples. All sampling was performed in triplicate by continuous venous aspiration after discarding the initial 2 mL of blood in contact with the internal jugular catheter. An average of all three readings was taken as a d-dimer level, provided no reading was > 10% from the other readings. In such eases, the > 10% outlier was discarded. This occurred in < 5% of blood samples drawn.
Time-Response Sampling
Two swine were utilized in this portion of the study to determine the time-response characteristics of t-PA bolus in the presence of an in situ clot. After 4 mg of IV t-PA, samples were obtained at 15-min intervals and analyzed (Fig 2).
Dose-Response Sampling
Once we established the optimal timing of t-PA effect, we proceeded to develop dose-response curves using five swine (Fig 3). Four preclot d-dimer samples were obtained. A femoral vein clot was created in situ, and plasma d-direct levels were measured every 15 min for 1 h to assess clot stability prior to IV t-PA administration. The d-dimer signal was then checked in triplicate 30 min after each escalating dose of t-PA; again, outliers were discarded as noted above.
Statistical Analysis
Analysis of variance was performed to assess for differences in D-dimer levels at baseline, after clot formation without t-PA, and alter t-PA boluses. When significant differences were established, paired t tests were performed between baseline vs clot without t-PA and after each incremental dose of t-PA. Significance was established at [alpha] = 0.05 level (p < 0.05).
RESULTS
Prior to administration of the t-PA bolus, baseline plasma d-dimer levels for preinstrumentation and postinstrumentation samples were stable (Fig 4, left, A). After the clot was formed in situ and the ligatures were released, no significant changes in plasma d-dimer levels were observed for 60 min (Fig 4, right, B). Time-response curves for the d-direct signal in two swine are shown in Figures 5 and 6. Both pigs showed a maximal response at 30 min. Thus, we chose 30 min after IV t-PA bolus as the sampling time in the escalating dose-response stage of the study (Fig 3). Elevation of d-dimer level with each escalating dose of exogenous t-PA occurred in all pigs, with significant changes occurring at the two highest doses (0.8 mg and 4 mg) [p < 0.03 and p < 0.003, respectively]. Figure 7 presents individual dose-response curves. A cumulative dose-response curve is displayed in Figure 8.
[FIGURES 4-8 OMITTED]
DISCUSSION
There are three major findings of our study. The first is that there is no significant change in the plasma d-direct signal over preinstrumentation and postinstrumentation baseline levels and during the first 60-min postclot formation (Fig 4). We attribute this to careful instrumentation technique, which avoided excessive tissue injury.
We cannot be certain that the clot totally occluded the femoral vein in each swine, since we did not cheek for patency after clot formation. However, the rubbery consistency of the clot suggested complete vessel occlusion. The striking consistency of the data over the 15-min interval prior to and after clot formation in all seven swine confirms the reliability of this finding, that acute in situ femoral clot does not elevate d-dimer signal.
One can only speculate if such a situation also occurs in human disease. Preliminary data suggest that this may be so in elderly and asymptomatic patients who appear to have lower endogenous t-PA levels. (7,8) In these circumstances, a d-dimer test result would not be expected to be positive, since the test requires not only mature clot formation with fibrin cross-stranding but also clot breakdown to its dimeric forms, which is the basis of the antigen-antibody reaction measured. (9) In these instances, neither latex nor ELISA tests would be of value unless enough clot breakdown occurs to elevate the signal above background noise. If this is proven to be the situation for clot formation ill the lower limbs in some humans, then the role of exogenous low-dose thrombolytics in amplifying the d-dimer signal would be crucial in making any d-dimer test (ELISA or latex) more sensitive.
Further, postoperative orthopedic patients have been shown to have low sensitivity of the latex d-dimer test for postoperative deep vein thrombosis. (10,11) These patients also have even fewer clinical symptoms of deep vein thrombosis. We believe this group might benefit from the "provoked d-dimer" assessment as well.
The second finding of our study shows that peak effect of bolus t-PA administration occurs by 30 min (Fig 4, 5). This is an acutely formed, lower-limb, deep vein thrombosis model, which would be expected to respond earlier and more promptly to exogenous t-PA bolus injection than a more chronic, and hence more organized, clot. The latter may relate to the clinical situation in which humans may present at varying times after clot formation. As such, the time-response assessment may be different in the overall human clinical population with suspected deep vein thrombosis. In any event, our study suggests that a wait of at least 30 min after t-PA bolus is required to detect the increase in d-dimer signal. Of course, more fibrin-specific thrombolytic agents such as tenecteplase may have an advantage over t-PA in this regard. Such differences, however, are entirely speculative at this point in time, until appropriate relevant studies are performed.
The third finding of our study is that a graded increase in d-dimer signal can be achieved with a minidose exogenous t-PA bolus after in situ clot formation (Fig 6, 7). In swine, at least 0.8 mg of t-PA is required to achieve a significant response in latex d-dimer signal.
Besides increasing the sensitivity of the d-dimer test for deep vein thrombosis, there may be an opportunity to reduce false-positive results and hence improve the specificity and positive predictive value of the d-dimer test. If positivity is due to high background noise unrelated to clot formation, then exogenous t-PA should not elevate the d-dimer signal in such instances. Of course, one has to be careful because other situations associated with diffuse intravascular clotting, such as hemolytic uremic syndrome or thrombotic thrombocytopenic purpura, could be responsible for the increase in d-dimer signal with t-PA, even when deep vein thrombosis is not present.
Several investigators have incorporated the d-dimer test with clinical probability and with other anatomic tests for clot presence to improve the positive predictive value for venous thromboembolism. Studies by the McMaster group have combined impedance plethysmography with the d-dimer test, showing an enhanced positive predictive value when results of both tests are positive. (12) Similarly, combining the d-dimer test with an indeterminate lung scan increases the positive predictive value for venous thromboembolism significantly. (13) Enhancing clot breakdown in cases where a clot has formed and insufficiently broken down may improve the clinical utility of the plasma d-dimer estimation in diagnosing thromboembolic disease.
Limitations of the Study
It is important to point out certain limitations of the current study. Our time-response measurements were made only in two swine. It is unlikely, however, in this acute in situ clot preparation that performing further time-response studies would have altered the findings of our study, as the goal was simply to establish a consistent sampling interval at a time which approximated to the peak t-PA effect on plasma d-dimer signal. An inappropriate choice of timing for d-dimer testing after t-PA bolus administration could have resulted in a false-negative result, which did not occur in our experiment. However, greater effort at time-response characterization needs to be performed in the clinical human populations presenting with suspected deep vein thrombosis.
Theoretically, doses of t-PA used to create a dose-response curve should have been randomized. This would, however, compromise the preparation by prolonging the experiment and/or the number of animals needed to obtain useful results. In the individual response curves (Fig 6), one can see complete congruence of the findings with progressively increasing d-dimer signal with each incremental dose of t-PA. For this reason, this is perhaps not a limitation but rather efficient use of laboratory animals to achieve an interpretable result using the smallest number of animals. Another limitation is the lack of overall time controls, such as following up animals without t-PA and without a clot for the duration of our experimental protocol to ensure that no time-related changes in d-dimer signal levels would occur. As this is an acute intervention study, we believed that the two 1-h periods before and after clot formation were adequate to establish clot stability (Fig 4). Similarly, with the intervention of exogenous t-PA, we had no "no-clot" controls with animals that had no clots induced but received t-PA. We chose not to perform no-clot controls, as we reasoned that if exogenous t-PA elevated the d-dimer signal in a no-clot animal, the most obvious cause would be break down of other sequestered clot in this acutely surgically instrumented animal. Such no-clot responses would not contribute to experimental clarity unless a reliable method for whole animal clot surveillance was available. This was not the case; hence, we did not perform these readings. Whether this limitation would have altered the interpretation of these very consistent and congruent findings in individual animals is unknown.
CONCLUSION
Acute, in situ femoral vein thrombosis is not associated with any increase in plasma d-dimer signal using a latex assay for 1 h after clot formation. In this acute, in situ clot preparation, exogenous minidose t-PA bolus increased d-dimer signal maximally at 30 rain alter bolus. A graded increase in d-dimer signal in swine with in situ femoral vein thrombus was seen starting at 0.03-mg bolus of t-PA and increasing with fivefold increments up to 4 mg. This becomes statistically significant at doses of 0.8 mg and 4 mg IV t-PA bolus (p < 0.03 and p < 0.003, respectively). Implications for this provoked d-dimer signal in assessment of humans with suspected deep vein thrombosis have been discussed.
ACKNOWLEDGMENT: We thank Dr. Casimir Eubig, Stella Reece, Maribeth Johnson, and Dr. Rhea-Beth Markowitz.
* From the Department of Medicine and Radiology (Dr. Robinson), Medical College of Georgia and Veterans Affairs Medical Center, Augusta, GA; Department of Internal Medicine (Dr. Pineda), University of South Carolina Medical Center and Veteran's Affairs Medical Center, Columbia, SC; Department of Internal Medicine (Dr. Salah), Medical College of Georgia, Augusta, GA; Department of Pediatric Surgery (Dr. Pipkin), University of Alabama, Birmingham, AL; Department of Radiology (Mr. Corley), Medical College of Georgia Augusta CA. Department of Clinical Pathology (Ms. Jonah) Medical College of Georgia, Augusta, GA; and Department of Internal Medicine (Dr. Gossage), Medical College of Georgia and Veterans Affairs Medical Center, Augusta, GA.
REFERENCES
(1) Anderson FA, Wheeler HB, Goldberg RJ, et al. A population based perspective of the hospital incidence and case-fatality rates of deep venous thrombosis pulmonary embolism: the Worcester study. Arch Intern Med 1991; 151:933-938
(2) Sandier DA, Martin JF. Autopsy proven pulmonary embolism in hospital patients: are we detecting enough deep vein thrombosis? J R Soc Med 1989; 82:203-205
(3) Jansen MC, Heebels AE, De Metz M, et al. Reliability of five d-dimer assays compared to ELISA in exclusion of deep venous thrombosis. Thromb Haemost 1997; 77:262-266
(4) Kearon C, Ginsberg JS, Donketis J, et al. Management of suspected deep vein thrombosis in outpatients by using clinical assessment and d-dimer testing. Ann Intern Med 2001; 135:108-111
(5) Kencht MF, Heinrich F. Clinical evaluation of an immunoturbidimetric d-dimer assay in the diagnostic procedure of deep vein thrombosis and pulmonary embolism. Thromb Res 1997; 88:413-417
(6) Kelly J Hunt BJ. Role of d-dimer in the diagnosis of venous thromboembolism. Lancet 2002; 359:456-457
(7) Bounameaux H, De Moerloose P, Perrier A, et al. Plasma measurement of d-dimer as diagnostic aid in suspected venous thromboembolism. Thromb Haemost 1994; 71:1-6
(8) Lee AY, Julian JA, Levine MN, et al. Clinical utility of a rapid whole blood d-dimer assay in patients with cancer who present with suspected acute deep venous thrombosis. Ann Intern Meal 1999; 131:417-423
(9) Crippa L, D'Angelo SV, Tomassini L, et al. The utility and cost-effectiveness of D-dimer measurements in the diagnosis of deep vein thrombosis. Haematologica 1997; 82:446-451
(10) Wattrisse G, Lecoutre D, Dufossez F, et al. Detection thromboembolique orthopedie traumatologie: interet et du dosage du D-dimere par la methode au latex. Cah Anesthesiol 1993; 41:130-134
(11) Deprost D, Ollivier V, Vie P, et al. D-dimer and thrombin-antithrombin III complex levels uncorrelated with phlebographic findings in 11 total knee replacement patients. Ann Biol Clin (Paris) 1990; 48:235-238
(12) Ginsberg J, Kearon C, Douketis J, et al. The use of d-dimer testing and impedance plethysmography examination in patients with clinical indications of deep vein thrombosis. Arch Intern Med 1997; 157:1077-1081
(13) Harrison KA, Haire WD, Pappas A, et al. Plasma d-dimer: a useful tool for evaluating suspected pulmonary embolus. J Nucl Med 1993; 34:896-898
The t-PA used in this study was provided by Genentech Inc., South San Fransisco, CA.
Manuscript received December 11, 2003; revision accepted September 7, 2004.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Vincent J. B. Robinson. MD, Medical College of Georgia Section of Cardiology, BBR 6515A, Department of Medicine, Augusta, GA 30912; e-mail: vrobinso@mail.mcg.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group