Melanoma is the third most common cancer to metastasize to the brain. Due to the extremely poor prognosis (median survival is often less than 6 months) and lack of effective therapy, patients are often excluded from clinical trials.
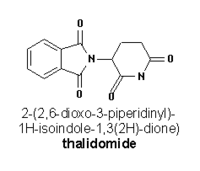
However, melanoma is a highly vascularized tumor, suggesting a possible role for an antiangiogenic agent in combating metastasis. Thalidomide has been shown to possess antiangiogenic properties. Preliminary research indicates that the combination of thalidomide and temozolomide--an oral congener of dacarbazine (DTIC)--may offer improved therapy for advanced melanoma.
Current Treatment
Chemotherapy and immunotherapy remain the primary treatments fur metastatic melanoma. Currently, DTIC is the only FDA-approved chemotherapeutic treatment. Response rates are often under 20 percent, with less than 5 percent of patients achieving a complete response. In addition, DTIC must undergo hepatic activation by the active metabolite monomethyl triazenoimidazole carboxamide (MTIC), and cannot cross the blood-brain barrier, so it is ineffective for patients with hepatic dysfunction or CNS metastases.
Actions of Temozolomide
Unlike DTIC, temozolomide does not require hepatic activation, and readily penetrates the blood-brain barrier. It is a prodrug that hydrolyzes to MTIC at physiologic pH. MTIC is the active metabolite of both temozolomide and DTIC, causing alkylation of DNA and inhibiting tumor growth.
The complete oral bioavailability of temozolomide and its ability to cross the blood-brain barrier make it an attractive alternative to DTIC. Results from a large randomized study in patients with metastatic melanoma have shown that the activity of temozolomide is similar to that of DTIC when administered on a 5-day dosing schedule.
As shown by Brock et al, a twofold increase in drug exposure could be achieved when temozolomide was administered on an extended continuous daily schedule. Continuous dosing with temozolomide might improve its antitumor activity by depleting a DNA repair enzyme involved in the tumor's drug resistance. It may also decrease the opportunity for tumor resistance.
Combining Temozolomide and Thalidomide
Whereas temozolomide works as a cytotoxic therapy, thalidomide has a cytostatic effect. Many of its biologic modulatory properties might have some therapeutic impact on melanoma. One or more of these activities may cause cytostasis and inhibit tumor growth. When administered in combination with cytotoxic chemotherapy, cytostatic therapy may inhibit tumor regrowth, development of resistant disease, and further metastases.
In October 1999, our group began using this combination to treat melanoma patients with brain metastases on a compassionate basis. Through December 2000, 16 patients (median age 57 years) had been treated. Objective responses were observed in seven patients: four complete responses (CRs) for all visible tumors and three partial responses (PRs), with at least 50 percent of all visible tumors having disappeared. Median survival was nine months (range 3-34+ months), with a median follow-up time of 22+ months in the four survivors. Historically, median survival for such patients is 3-4 months.
Phase II Study
Based on these encouraging results, we conducted a phase II study of this combination therapy to establish its efficacy in metastatic melanoma patients with and without brain metastasis. Temozolomide was administered on a continuous daily dosing schedule for six weeks at 75 mg/m2/day with a two-week break between cycles. Patients < 70 years old began thalidomide at 200 mg/day; the dose was escalated by 100 mg/day at two-week intervals to a maximum of 400 mg/day. Patients > 70 years old began thalidomide at 100 mg/day, with 50 mg/day increments at two-week intervals up to a maximum of 250 mg/day. The response was evaluated every eight weeks.
Preliminary results for the 38 patients without brain metastases have recently been reported. Tumor regression was observed in lung, liver, and soft tissue, with objective responses in 12 patients (31.6 percent--one CR and 11 PRs). The median overall survival for the entire cohort thus far is 9.5 months; 5.9 months for nonresponders and has not yet been reached for the 12 responders (p = 0.02). The most frequent non-hematologic toxicities have included rash, constipation, vomiting, fatigue, dizziness, dyspnea, nausea, headache, non-neutropenic infection, edema, tremor, and drowsiness; most toxicities have been grade 2. Grade 3 lymphopenia occurred in 14 patients; < 10 percent of patients showed other grade 3 hematologic toxicities.
This level of toxicity is mild compared to the most aggressive biochemotherapy, where the common toxicities are often grade 4 and hospitalization is required for administration. The effectiveness of this regimen also appears to compare favorably with phase III studies of either combination chemotherapy or biochemotherapy, where no survival benefit has been demonstrated.
Our other study cohort, patients with brain metastases, is ongoing. To date, 21 patients have been enrolled; only 13 have received at least one cycle of therapy. Five objective responses in the brain have been observed--three CRs and two PRs. In general, this combination therapy is well tolerated, even in elderly patients who are not suitable candidates for more toxic regimens.
A confirmatory multicenter Phase II study in large numbers of patients with brain metastases will be initiated by the Melanoma Working group at Cancer and Leukemia Group B in 2003.
Conclusion
Complete responses are rare in stage IV melanoma, particularly in patients with brain metastases; a high proportion of these patients die from complications of the brain metastases. Thus, the responses achieved to date with combination temozolomide and thalidomide are extremely encouraging. They offer the potential prospect of an effective therapy, long-term control of metastatic melanoma, and significantly improved patient outcome.
References
Wen PY, Black PM, Loeffler JS. Treatment of metastatic cancer. In: DeVita VT Jr., Hellman S, Rosenberg SA (eds): Cancer: Principles & Practice of Oncology. 6th ed., Philadelphia, PA: Lippincott, Williams & Wilkins 2001; 2655-2670.
D'Amato RJ, Michael S, Loughnan EF, Folkman J. Thalidomide is an inhibitor of angiogenesis. Proc Natl Acad Sci USA 1994; 91:4082-4085.
Middleton MR, Grob JJ, Aaronson N, Fierlbeck G, Tilgen W, Seiter S, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic melanoma. J Clin Oncol 2000; 18:158-166.
Brock CS, Newland ES, Wedge SR, Bower M, Evans H, Colquhoun I, et al. Phase I trial of temozolomide using an extended continuous oral schedule. Cancer Res 1998; 58:4363-4367.
Hwu WJ, Raizer J, Panageas KS, Lis E. Treatment of metastatic melanoma in the brain with temozolomide and thalidomide. Lancet Oncol 2001; 2:634-635.
Hwu WJ, Krown SE, Menell JH, Panageas KS, Merrell J, Quinn CJ, et al. Temozolomide (TMZ) plus thalidomide in patients with advanced melanoma: a phase II trial. Proc Am Soc Clin Oncol 2002; 21:344a, Abstract 1372.
WEN-JEN HWU, MD, PHD
DEPARTMENT OF MEDICINE, MEMORIAL SLOAN-KETTERING CANCER CENTER, NEW YORK, NEW YORK
COPYRIGHT 2003 Journal of Drugs in Dermatology
COPYRIGHT 2003 Gale Group