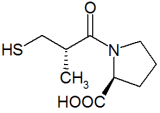
Study objectives: To determine whether captopril (CAP) therapy had an effect on the minute ventilation/carbon dioxide output (VE/[VCO.sub.2]) ratio at submaximal levels of exercise in asymptomatic patients with reduced left ventricular function after myocardial infarction.
Design: Double blinded, randomized, prospective, repeated measures.
Patients and interventions: One hundred thirty-five patients with left ventricular ejection fractions of [is less than] 40% were randomly assigned to a treatment group (CAP; n = 62) or a placebo group (PLC; n = 73). Subjects had cycle ergometer exercise tests at 2 to 6 months (T1), 10 to 14 months (T2), and [is greater than] 22 months (T3) postmyocardial infarction.
Measurements: Oxygen uptake ([VO.sub.2]), [VCO.sub.2], and VE were measured throughout each exercise test. Dependent variables were peak [VO.sub.2] ([VO.sub.2] peak), the ventilatory anaerobic threshold (VAT), and the VE/[VCO.sub.2] ratio measured at 30 W and at 75% [VO.sub.2] peak.
Results: [VO.sub.2] peak and VAT did not differ as a result of treatment (CAP vs PLC; p = 0.92 and 0.80) or over time (T1 vs T2 vs T3; p = 0.51 and 0.07). VE/[VCO.sub.2] was significantly lower for CAP at 30 W (p = 0.05) and, although lower at 75% [VO.sub.2] peak, did not obtain statistical significance (p = 0.22). The between group differences were larger at T2 and T3 when compared with TI.
Conclusions: CAP resulted in a reduced VE/[VCO.sub.2] ratio during submaximal exercise. The reduced ventilation may permit patients to perform their normal activities of daily living at a lower perception of difficulty, reduce symptoms, and provide an improved quality of life.
(CHEST 1998; 114:1289-1294)
Key words: angiotensin-converting enzyme inhibitors; carbon dioxide output; minute ventilation; oxygen uptake; postmyocardial infarction
Abbreviations: ACE = angiotensin-converting enzyme; ANOVA = analysis of variance; CAP = captopril; PLC = placebo; T1 = 4-month test; T2 = 12-month test; T3 = 24-month test; VAT = ventilatory/anaerobic threshold; VE/[VCO.sub.2] = minute ventilation/carbon dioxide output (ventilatory equivalent for oxygen); [VO.sub.2] = oxygen uptake
The pharmacologic actions of angiotensin-converting enzyme (ACE) inhibition that may contribute to an increased exercise tolerance may be more effective at submaximal levels of exercise than at peak exercise. The impact of ACE inhibition on peak exercise capacity has been varied.[1-5] For peak exercise capacity to be enhanced, maximal cardiac output, maximal oxygen utilization, or both must be increased.[6,7] For patients with poor left ventricular function and a limited cardiac reserve, ACE inhibitors may not be effective for improving peak exercise capacity. There may be, though, a reduction in ventilation at submaximal levels of exercise when there remains a residual cardiac reserve (cardiac reserve and oxygen utilization have not been maximized). The reduced afterload caused by ACE inhibition may result in an improved central hemodynamics, vasodilator reserve, increased muscle blood flow, and possible changes in muscle energetics. These changes may result in a lower anaerobic contribution to energy production and a reduced lactate accumulation. Subsequent to these changes, there may be a reduction in the ventilatory equivalent for carbon dioxide (minute ventilation/carbon dioxide output [VE/[VCO.sub.2]) during submaximal exercise.[8,9]
ACE inhibitors may lower the VE/[VCO.sub.2] ratio at matched absolute (below the anaerobic threshold) and relative (percentage of peak exercise capacity) workloads. The VE/[VCO.sub.2] at submaximal workloads is easier to measure than peak oxygen uptake ([VO.sub.2] peak) and is not reliant on a subjective voluntary effort. The VE/[VCO.sub.2] serves as a simple and objective measure of the severity of symptoms associated with exercise and as a marker of improved exercise tolerance.[10,11] From the patient's point of view, the ability to perform continuous submaximal exercise at a reduced perception of effort is more important than peak force generation.[12] The practical significance of a reduced VE/[VCO.sub.2] at submaximal workloads includes an enhanced ability to perform normal activities of daily living, recreation, and occupational tasks at a reduced ventilatory demand and reduced feelings of breathlessness. These adaptations may contribute to the documented overall improvement in quality of life associated with ACE inhibition therapy.[13] The reduced VE/[VCO.sub.2] may help explain the subjective improvement in symptoms of heart failure noted by patients and documented by their physicians when ACE inhibition therapy is given.
The purpose of this investigation was to determine whether captopril (CAP) therapy had an effect on the VE/[VCO.sub.2] at submaximal levels of exercise in asymptomatic patients with reduced left ventricular function for up to 24 months following a myocardial infarction.
MATERIALS AND METHODS
Subjects
Subjects were recruited and enrolled from five centers as described in the SAVE (Survival After Ventricular Enlargement) ancillary exercise trial.[1] Patients had no active angina and were able to perform upright cycle exercise. A total of 135 patients were randomly assigned to a treatment group who received CAP (n = 62) or a placebo (PLC) n = 73). Both patients and investigators were blinded as to whether they were in the CAP or PLC group. CAP dosage was gradually increased to a maximum of 50 mg three times daily unless the physician or the patient attributed any adverse experience to the therapy. Demographic data, infarct characteristics, and medications for the current study population are presented in Table 1.
(*) There were no significant between group differences (p > 0.05). LVEF = left ventricular ejection fraction. Values are means [+ or -] SDs.
Exercise Tests
Cycle ergometer tests were performed at 3 to 6 months (4-month test; T1), 10 to 14 months (12-month test; T2), and [is greater than] 22 months (24-month test; T3) postmyocardial infarction. The initial 3-rain workstage of 15 W was increased to 30 W with 30-W increments every 3 min thereafter until fatigue occurred. [VO.sub.2], [VCO.sub.2], and VE were recorded continuously throughout the test using standard open circuit spirometric procedures. Twelve-lead ECGs and BP were monitored by standard procedures for patient safety. The [VO.sub.2] peak was the largest value for [VO.sub.2] obtained during exercise. Tests were terminated at the point of volitional fatigue or breathlessness. Subjects were encouraged to continue as long as possible. The ventilatory anaerobic threshold (VAT) was calculated from the plots of VE against carbon dioxide.[14] The VE/[VCO.sub.2] ratio was calculated as the VE (BTPS; mL/min) divided by [VCO.sub.2] (STPD; mL/min) at the third minute of exercise at 30 W and at 75% [VO.sub.2] peak.
Complete data sets were obtained at 30 W (completed the entire 3 rain at 30 W) for 116 patients at T1, 100 at T2, and 97 at T3. Incomplete data sets occurred for the following reasons: died before testing could be completed, equipment failure, patient refusal, miscellaneous medical problems, changes in residence, incomplete ventilatory data for each work stage, and test termination before 30 W were completed. Forty-one PLC group and 34 CAP patients had complete data sets for all three tests at 30 W. Forty-eight PLC and 41 CAP patients had complete data sets at 75% [VO.sub.2] peak. Forty-eight PLC and 42 CAP had complete data sets for all three tests for [VO.sub.2] peak and 23 PLC and 18 CAP for VAT. The number of patients completing each test for each dependent variable can be found in the tables.
Data Analysis
A one-way analysis of variance (ANOVA) and Kruskal-Wallis one-way ANOVA on ranks compared between-group demographics (SigmaStat Statistical Software; Jandel Scientific, Jandel Corporation; San Rafael, CA). A two-way ANOVA with repetition was computed to determine the level of significance for any group (PLC vs CAP), time (T1 vs T2 vs T3), or interaction effect for [VO.sub.2] peak, VAT, and VE/[VCO.sub.2] at 30 W (Fig 1), and 75% [VO.sub.2] peak (Fig 2). This analysis included only patients who completed all three tests. A one-way ANOVA and Kruskal-Wallis one-way ANOVA on ranks (nonnormally distributed data) were computed to determine group (PLC vs CAP) effects for each test, including all patients who completed that specific test. This was performed to help assess any potential impact of patient dropout on group differences.
[Figures 1-2 ILLUSTRATION OMITTED]
All data are presented in the tables and graphs using means and SDs (tables) or mean SEs (figures).
RESULTS
There were no demographic differences between groups and the groups were following a similar medical regimen (Table 1). Figures 1 and 2 illustrate data for those completing all three tests with complete sets of data at 30 W (n = 75) and 75% [VO.sub.2] peak (n = 99). The tables contain the data for all those who completed each test.
[VO.sub.2] peak (mL/min) did not differ as a result of treatment (CAP vs PLC; p = 0.92) or time (T1 vs T2 vs T3; p = 0.51) (Table 2). VAT (mL/min) did not differ as a result of treatment (CAP vs PLC; p = 0.80) or time (T1 vs T2 vs T3; p = 0.07).
(*) [VCO.sub.2] increased from T1 to T3 (p = 0.044) with no other group, time, or interaction effects at the p < 0.05 level. RQ = respiratory exchange ratio.
At 30 W, there was a significant group (p = 0.05) and time (p = 0.06) effect for VE/[VCO.sub.2]. VE/[CO.sub.2] decreased with time in CAP patients but remained the same from T1 thru T3 for PLC patients (Fig 1; Table 3). There was a significant group and time interaction for VE (p = 0.06) with VE being greater for CAP patients at T1 (28.9 vs 27.9 L/min) but lower for CAP patients for T2 (26.7 vs 27.4 L/rain) and T3 (26.9 vs 27.8 L/rain). [VO.sub.2] showed no group (p = 0.17), time (p = 0.79), or interaction (p = 0.023) effects (Table 3). There were no group, time, or interaction effects for [VCO.sub.2] (p = 0.16, 0.94, and 0.65, respectively).
(*) VE/[VCO.sub.2] was greater for PLC at T3 (p = 0.016; Fig 1). There were no other group, time, or interaction effects at the p < 0.05 level. VE/[VO.sub.2] = ventilatory equivalent for oxygen. See Table 2 footnote for explanation of RQ.
The VE/[VCO.sub.2] at 75% [VO.sub.2] peak appeared to parallel the differences at 30 W being lower in the CAP group, particularly at T2 and T3. The differences, though, did not obtain statistical significance for group (p = 0.22), time (p = 0.25), or interaction (p = 0.58) (Fig 2; Table 4). There were no significant group (p = 0.46), time (p = 0.08), or interaction (p = 0.26) effects for VE. [VO.sub.2] demonstrated a significant interaction effect (p = 0.04), being lower at T2 for CAP patients (992 mL/min) vs PLC patients (1,082 mL/min). [VO.sub.2] was similar between CAP and PLC patients for T1 (999 vs 970 mL/min) and T3 (1,046 vs 1,085 mL/min). There were no significant effects for [VCO.sub.2] for group (p = 0.99), time (p = 0.08), or interaction (p = 0.29).
(*) There were no group, time, or interaction effects at the p < 0.05 level. See Table 2 and 3 footnotes for explanations of abbreviations.
DISCUSSION
Submaximal Exercise
CAP therapy decreased the VE/[VCO.sub.2] at submaximal levels of exercise. The differences appeared to increase with time (greatest at T2 and T3 vs T1). The elevated VE/[VCO.sub.2] during exercise in those with impaired cardiac function has been attributed to the following: (1) impaired central hemodynamics; (2) reduced pulmonary blood flow; (3) ventilation/ perfusion mismatching; (4) flow restrictions to the peripheral skeletal muscles; or (5) changes in the muscle fiber morphology or oxidative capacity. These changes increase the anaerobic contribution to energy production during exercise and result in an increased lactate production and an increased buffering induced VE.[10-12,15,16] Dyspnea could also result from respiratory muscle changes, such as increased diaphragmatic work and accessory muscle oxygenation[17,18] and reduced respiratory muscle strength. [19,20] In that the VE/[VCO.sub.2] slope is steeper in congestive heart failure patients and that the relationship is nonlinear suggests that there may also be a non-[CO.sub.2] signal for ventilation that is enhanced in heart failure (ie, muscle ergoreflex,[21] central command,[22] or potassium,[23] and other noncarbon dioxide, non-pH metabolic factors[12]).
The afterload reducing properties of ACE inhibition have the potential to improve muscle blood flow, oxygen utilization abnormalities,[8,9,13,16] and subsequently reduce VE during exercise. Central improvements with ACE inhibitors are rapid, but increases in exercise capacity are delayed for weeks or months.[24] This is consistent with the current findings in that the differences in VE/[VCO.sub.2] between CAP patients and PLC patients became greater with time (greater at T2 and T3 vs T1) (Figs 1 and 2). The delayed improvement in exercise capacity seen after treatment with ACE inhibitors is associated with the increase in leg blood flow and the correction of muscle metabolic abnormalities.[25] These improvements are most evident for therapies associated with a specific improvement in muscle function or in exercise performance[26] and suggest that the limiting factor to exercise tolerance is not the capacity to deliver oxygen to the exercising muscle, but it is the capacity of the exercising muscle to consume [O.sub.2].
A treatment-induced reduction in VE/g[CO.sub.2] would suggest that a selected level of exercise could be performed at a lower ventilatory stress. Therefore, symptoms and the patient's perception of effort necessary to perform physical tasks may also improve.[13] These improvements may allow the patient to perform their activities of daily living more comfortably and improve their overall perception of quality of life.
[VO.sub.2] peak
There have been disparate findings as to whether ACE inhibition improves peak exercise capacity. Investigators have found no change in exercise capacity as a result of ACE inhibition when compared with PLC groups while others have reported increases in exercise capacity apparently attributed to ACE inhibition therapy. The current PLC group demonstrated an increase in [VO.sub.2] peak of 5.7% from T1 to T2 but a decrease from T2 to T3 of -1.0%. The CAP group decreased from T1 to T2 (-3.9%) but then increased from T2 to T3 (4.6%). Mancini and coworkers[4] found an overall increase in [VO.sub.2] peak of 15.7% in eight patients, but four of their patients had large increases whereas the remaining four patients had small increases; therefore, interpatient variability was large. Dickstein and Aarsland[2] found that enalapril resulted in a greater exercise capacity at 1 month after an acute myocardial infarction but the differences between the treatment and the PLC group was absent after 6 months of therapy. Dickstein and coworkers[3] found that long-term enalapril therapy (1 year) after a myocardial infarction did not result in an increase in exercise capacity when compared with the PLC group. The CAP Multicenter Research Group[5] used exercise time as their measure of exercise capacity and found that the CAP-treated group progressively increased their exercise time throughout 12 weeks of treatment. Symptoms of dyspnea, fatigue, and orthopnea also improved. Study review demonstrates that differences in experimental design may contribute to the disparate results. These differences include the length of the study, patient populations studied, and the type of exercise used for testing (treadmill vs cycle). Also, the measure of exercise capacity was different between studies. Some did not measure [VO.sub.2] but used exercise time as their measure of exercise capacity. Exercise time is more susceptible to familiarization than measures of [VO.sub.2] peak.
Physiologically, ACE inhibition may not increase peak exercise capacity in those with reduced left ventricular function. For improvements in peak exercise capacity to occur, either maximum cardiac output or oxygen extraction has to increase. The afterload reducing effect of CAP for patients who have a diminished cardiac reserve may not result in an enhancement of an already maximized cardiac output at peak exercise. Subsequently, peak exercise capacity will not increase. Wilson and coworkers[27] classified heart failure patients into those who had a preserved cardiac output response to exercise and those who had a reduced cardiac output response to exercise. The reduced cardiac output response group were limited by skeletal muscle underperfusion and unable to improve their [VO.sub.2] max with exercise training. The normal cardiac output responders showed improved [VO.sub.2] max values with exercise training. This is consistent with our findings since our patients (who did not improve their [VO.sub.2] peak) suffered from left ventricular dysfunction and may have had a reduced cardiac output response to exercise.
The afterload reducing effect of ACE inhibition during submaximal exercise, though, may improve ventilation in those with an impaired cardiac output response. In that a cardiac reserve may exist during submaximal exercise, cardiac output and muscle blood flow may increase as a result of the afterload reducing effects of CAP. This would reduce the required anaerobic contribution to energy production, decrease lactate production, and the buffering induced increase in VE. The reduced ventilatory demands may result in a reduced perception of effort during required and desired tasks of daily living, a lower incidence of symptoms, and an overall improvement in quality of life.
Study Limitations
This study was started before the possible adverse side effects of calcium channel blockers on postmyocardial infarction patients were known. Although the possibility cannot be totally ruled out that calcium channel blockers may have affected the outcome in this study, the similarity of distribution between the study groups (56% vs 48%) makes it seem unlikely to have been a significant confounding variable.
The present study may also have some subject bias. Only patients who completed all three tests were included in the initial analysis assessing group, time, and interaction effects. We cannot account for all deaths and dropouts completely; however, if the number of patients who died, dropped out, or had inadequate gas exchange data are considered (21 of 62 [34%] PLC patients and 39 of 73 [53%] CAP patients at 30 W and 14 of 62 [23%] PLC patients and 32 of 73 [43%] CAP patients at 75% [VO.sub.2] peak), the results may have been obscured by these losses. To account for this, data analysis was performed for each test individually using all patients who completed that specific test to assess for group differences.
CONCLUSIONS
Although there may be no differences in peak exercise capacity as a result of CAP therapy, there is a reduction in the VE/[VCO.sub.2] ratio at submaximal levels of exercise. The levels of exercise used approximate the energy demands of routine activities of daily living. From the patient's point of view, the ability to perform repeated or prolonged submaximal exercise is more important than peak force generation in that patients spend their normal daily routines performing tasks of a submaximal nature. The practical significance of these changes include an improved ability to perform normal activities of daily living and desired recreational and occupational tasks, reduced symptoms and perception of effort, and the documented improved quality of life associated with the use of ACE inhibitors.[13]
REFERENCES
[1] Hartley LH, Flaker G, Basta L, et al. Physical work capacity after acute myocardial infarction in patients with low ejection fraction and effect of captopril. Am Cardiol 1995; 76:857-860
[2] Dickstein K, Aarsland T. Effect of exercise performance of enalapril therapy initiated early after myocardial infarction. J Am Coll Cardiol 1993; 22:975-983
[3] Dickstein K, Barvick S, Aarsland T. Effect of long-term enalapril therapy on cardiopulmonary exercise performance after myocardial infarction. Circulation 1991; 83:1895-1904
[4] Mancini DM, Davis L, Wexler Jp, et al. Dependence of enhanced maximal exercise performance on increased peak skeletal muscle perfusion during long-term captopril therapy in heart failure. J Am Coll Cardiol 1987; 10:845-850
[5] Captopril Multicenter Research Group. A placebo-controlled trial of captopril in refractory chronic congestive heart failure. J Am Coll Cardiol 1983; 2:755-763
[6] Detry JMR, Rouseau M, Vandenbrouke G, et al. Increased arterial oxygen difference after physical training in coronary heart disease. Circulation 1971; 44:109-118
[7] Ehsani AA, Martin WH, Heath GW, et al. Cardiac effects of prolonged and intense exercise training in patients with coronary artery disease. Am J Cardiol 1982; 50:246-254
[8] Broqvist M, Dahlstrom U, Karlsson E, et al. Muscle energy metabolism in severe chronic congestive heart failure--effect of treatment with enalapril. Eur Heart J 1992; 13:1217-1224
[9] Timmis AD, Bojanowsky MR, Najm YC, et al. Captopril versus placebo in congestive heart failure: effects on oxygen delivery to exercising skeletal muscle. Eur Heart J 1987; 8:1295-1304
[10] Hachamovitch R, Brown HV, Rubin SA. Respiratory and circulatory analysis of [CO.sub.2] output during exercise in chronic heart failure. Circulation 1991; 84:605-612
[11] Lewis NP, MacDougall IC, Willis N, et al. The ventilatory cost of exercise compared in chronic heart failure and chronic renal anemia. Q J Med 1992; 84:423-531
[12] Clark AL, Poole-Wilson PA, Coats AJS. Exercise limitation in chronic heart failure: central role of the periphery. J Am Coll Cardiol 1996; 28:1092-1102
[13] Rector TS. Effect of ACE inhibitors on the quality of life of patients with heart failure. Coron Artery Dis 1995; 6:310-314
[14] Beaver WL, Wasserman K, Whipp BJ. A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 1986; 60:2020-2027
[15] Metra M, Dei Cas L, Panina G, et al. Exercise hyperventilation in chronic congestive heart failure and its relation to functional capacity and hemodynamics. Am J Cardiol 1992; 70:622-628
[16] Kraemer MD, Kubo SH, Rector TS, et al. Pulmonary and peripheral vascular factors are important determinants of peak oxygen uptake in patients with heart failure. J Am Coll Cardiol 1991; 21:641-648
[17] Mancini DM, Ferraro N, Nazzaro D, et al. Respiratory muscle deoxygenation during exercise in patients with heart failure demonstrated with near-infra-red spectroscopy. J Am Coll Cardiol 1991; 18:492-498
[18] Mancini DM, Henson D, LaManca J, et al. Respiratory muscle function and dyspnea in patients with chronic heart failure. Circulation 1992; 86:909-919
[19] Hammond MD, Bauer KA, Sharp JT, et al. Respiratory muscle strength in congestive heart failure. Chest 1990; 98:1091-1094
[20] McParland C, Krishnan B, Wang Y, et al. Inspiratory muscle weakness and dyspnea in chronic heart failure. Am Rev Respir Dis 1992; 146:467-472
[21] Tibes U. Reflex inputs to the cardiovascular and respiratory centers from dynamically working canine muscles. Circ Res 1977; 41:332-341
[22] Eldridge FL, Milhorn DE, Kiley JP, et al. Stimulation by central command of locomotion, respiration and circulation during exercise. Respir Physiol 1985; 59:313-317
[23] Paterson DJ, Robbins PA, Conway J. Changes in arterial plasma potassium and ventilation during exercise in man. Respir Physiol 1989; 78:323-330
[24] Wilson JR, Martin JL, Ferraro N, et al. Impaired skeletal muscle nutritive flow during exercise in patients with congestive heart failure: role of cardiac pump dysfunction as determined by the effect of dobutamine. Am J Cardiol 1984; 53:1308-1315
[25] Drexler H, Bahhardt U, Meinertz T, et al. Contrasting peripheral short-term and long-term effects of converting enzyme inhibition in patients with congestive heart failure: a double-blind, placebo-controlled trial. Circulation 1989; 79: 491-502
[26] Piepoli M, Clark AL, Volterrani M, et al. Contribution of muscle afferents to the hemodynamic, autonomic, and ventilatory responses to exercise in patients with chronic heart failure: effects of physical training. Circulation 1996; 93:940-952
[27] Wilson JR, Groves J, Rayos G. Circulatory status and response to cardiac rehabilitation in patients with heart failure. Circulation 1996; 94:1567-1572
(*) From the Department of Cardiology (Drs. McConnell and Menapace), Geisinger Medical Center, Danville, PA; and the Cardiovascular Division (Drs. Hartley and Pfeffer), Brigham and Women's Hospital, Boston, MA.
Manuscript received December 3, 1997; revision accepted June 1, 1998.
Correspondence to: Timothy R. McConnell, PhD, Director, Cardiac Rehabilitation, Geisinger Medical Center, Danville, PA 17822-2160; e-mail: tmcconnell@psghs.edu
COPYRIGHT 1998 American College of Chest Physicians
COPYRIGHT 2000 Gale Group