Introduction
The need to monitor the safety of new medicines in large populations of patients is well established,[1] particularly since an average of only 1480 patients is recruited into clinical trial programmes before a new drug is marketed.[2] It is only then that a comprehensive assessment of its safety can be made. Formal postmarketing surveillance conducted in broadly based clinical settings contributes to the evaluation of drug safety.[1]
A review of 31 postmarketing surveillance studies (conducted under the voluntary guidelines issued in 1987[3 4]) concluded that these had made only a limited contribution to the assessment of drug safety. The main criticisms were that patients were identified prospectively for inclusion, no comparison groups were used, and recruitment to the studies was slow. Furthermore, results were seldom published, so prescribers remained ignorant of the findings. To address these concerns, formal guidelines for the design of company sponsored safety assessment of marketed medicines were introduced in 1994 (table 1).[1]
Table 1 Main criticisms of postmarketing surveillance studies and recommendations to address these(1)
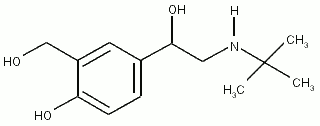
We conducted a postmarketing surveillance study of the first licensed, pressurised, metered dose inhaler to use a non-chlorofluorocarbon propellant--the hydrofluoroalkane 134a salbutamol sulphate inhaler (Airomir, 3M). The study complied with the safety assessment of marketed medicines guidelines.[1] Controlled trials had shown that metered dose salbutamol inhalers using hydrofluoroalkane as the propellant were comparable in terms of efficacy and safety to existing salbutamol inhalers using chlorofluorocarbon as the propellant.[5-8] We aimed to evaluate the safety of the hydrofluoroalkane inhaler in patients prescribed salbutamol in primary care by comparing it with an inhaler using chlorofluorocarbon as the propellant.
Methods
An independent steering committee was formed, as recommended by the guidelines. The committee's responsibilities included approving the study design, monitoring progress, and reviewing reports of adverse events.
Study design
An open label, non-randomised, non-interventional observational study design was chosen, with the aim of recruiting rapidly a large cohort of patients representative of the general population being treated with pressurised metered dose salbutamol inhalers. Normal clinical practice was followed. Neither the patient nor the doctor had to undertake any procedures related to the study. Patients did not have to make additional visits to the surgery. Recruitment of patients, therefore, reflected the general prescribing habits for salbutamol in relation to all the indications for which the drug had been licensed.
General practitioners
Altogether, 11 300 general practitioners throughout the United Kingdom were invited to participate. The letter of invitation described the rationale for replacing chlorofluorocarbon in metered dose inhalers, the design and objectives of the study, the predicted workload, the payment schedule, and the number of patients to be enrolled.
Patients
To generate a large population, patients were recruited in the ratio of one using a chlorofluorocarbon inhaler to five using a hydrofluoroalkane inhaler. They were considered for treatment with the hydrofluoroalkane inhaler only after the clinical decision to start or modify salbutamol treatment had been made. The first patient in each block of six continued using their existing chlorofluorocarbon inhaler, while the next five were prescribed the hydrofluoroalkane inhaler.
Data collection
Data were collected by the investigator from the patients' medical records for the three month study period. The quality of data was ensured by conducting source data verification on one randomly selected patient in each group of six patients at each centre.
Statistical methods
The planned sample size of 6468 subjects provided 80% statistical power to detect a relative risk of 2.0 for patients having at least one admission to hospital (for the condition for which salbutamol was prescribed) at a significance level of 5%. The underlying assumption was that the rate of hospital admission during the three months of the study would be not less than 1.25% in the group using chlorofluorocarbon inhalers.
Baseline characteristics relating to the severity of the condition being treated in each group were compared by computing odds ratios and associated 95% confidence intervals. Severity was inferred from the daily dose of inhaled steroids--[is greater than]800 [micro] g/day beclomethasone dipropionate or [is greater than] 400 [micro] g/day fluticasone propionate was considered to indicate a serious condition. Logistic regression analysis was used to analyse the rates of patient-doctor consultations (that is, hospital admission, attendance at accident and emergency units, unscheduled surgery visits, and unscheduled home visits). The effect of treatment was assessed after adjusting for the following covariates: sex, age, ethnic origin, severity, and duration of condition. The incidence of adverse events in each treatment group was compared using Fisher's exact test. Separate analyses were performed for individual adverse events, serious adverse events, and those probably or possibly related to study treatment.
Consent
The safety assessment of marketed medicines guidelines states that ethics committee approval is not required for a non-randomised, non-interventional study. However, patients did give written informed consent to information being extracted from their notes and used in the study.
Results
Altogether, 1223 general practitioners (10.8%) accepted the invitation to participate and 1096 confirmed their agreement after they had received a detailed description of the study. Six hundred and forty six of these general practitioners, widely distributed throughout the United Kingdom, participated and recruited a total of 6614 patients (5402 of whom were using a hydrofluoroalkane inhaler and 1212 a chlorofluorocarbon inhaler). The two groups were comparable in terms of age, sex, ethnic origin, and diagnosis (table 2). The first patient was enrolled on 21 May 1995 and the study was completed 15 months later.
Data for a few patients were unavailable.
Admissions and consultations
There was no appreciable difference between the groups in the rate of hospital admissions attributable to the condition for which salbutamol had been prescribed (hydrofluoroalkane inhaler 2.3% and chlorofluorocarbon inhaler 3.1%; odds ratio 0.75 (0.51 to 1.08)) (table 3). Multivariate analysis--adjusting for age, sex, ethnic origin, disease duration, and severity--showed no statistically significant differences (odds ratio 0.84 (0.58 to 1.23)).There were no appreciable differences between the groups in the proportions of patients who attended accident and emergency departments, made unscheduled visits to the surgery or had home visits (table 3).
(*) Adjusted for effects of sex, age, ethnic origin, duration, and severity of disease.
Adverse events
General practitioners recorded adverse events in similar proportions of patients in each group (24.8% hydrofluoroalkane inhalers and 24.5% chlorofluorocarbon inhalers; odds ratio 1.01 (0.88 to 1.17)) (table 4). The most commonly reported adverse affects were infection, bronchospasm, and upper respiratory tract infection. General practitioners attributed more adverse events to hydrofluoroalkane inhalers (3.1%) than to chlorofluorocarbon inhalers (0.7%). No deaths were attributable to the condition for which salbutamol had been prescribed or to the study medications. The incidence of serious adverse events was higher in patients using chlorofluorocarbon inhalers (3.7%) than in those using hydrofluoroalkane inhalers (2.7%) (table 4).
Withdrawal from the study
Overall, more patients using the hydrofluoroalkane inhaler withdrew from the study. (P [is less than] 0.001) (table 5). Most patients in both groups (10.4% hydrofluoroalkane inhaler and 3.1% chlorofluorocarbon inhaler) withdrew for reasons unrelated to safety. These included intercurrent illness, lost to follow up, and inadvertent prescription errors. In the hydrofluoroalkane salbutamol group, 3.1% patients withdrew because they disliked the taste. More patients using the hydrofluoroalkane inhaler stopped taking study medication because of adverse events (3.8% compared with 0.2% in the chlorofluorocarbon inhaler group). The proportion of patients who stopped using the hydrofluoroalkane inhaler because of adverse events fell from 1.9% during the first 30 days to 0.7% between days 61 and 90. Over 80% of patients in both groups completed three months of treatment with the study medication.
(*) P < 0.001.
Discussion
We describe a non-interventional, non-randomised observational study undertaken to document early postmarketing experience with a metered dose salbutamol aerosol inhaler using hydrofluoroalkane as the propellant. The study is unusual in that it evaluated the reformulation of an existing drug in a new propellant system. It aimed to evaluate the safety of a hydrofluoroalkane inhaler by comparing it with existing chlorofluorocarbon inhalers in patients prescribed salbutamol in primary care. We believe that this is the first postmarketing surveillance study conducted under safety assessment of marketed medicines guidelines to be submitted for publication.
The study met the objectives of the safety assessment of marketed medicines guidelines and also fulfilled standards laid down in the European Agency for the Evaluation of Medicinal Products' guidelines for postmarketing surveillance studies on nonchlorofluorocarbon metered dose inhalers, which came into effect while the study was in progress (table 6)) The use of these guidelines in this and future trials is expected to increase the credibility of postmarketing surveillance studies.
The response rate of general practitioners to the invitation to participate in the study was high (10.8%). Conventional wisdom regarding large mailshots suggests that a response rate between 5% and 8% is usual.
The study highlighted several differences in study design or conduct and outcome between a postmarketing surveillance and randomised controlled trials. To ensure broad comparability between the groups, control patients were recruited at the same time from the same general practices as the patients using the hydrofluoroalkane inhalers. Nonetheless, because of the open nature of the study, it was anticipated that there would be differences between groups in, for example, adverse events attributable to treatment. We used the number of patients who had been admitted to hospital at least once for the condition for which salbutamol had been prescribed as the primary outcome variable. This provided an objective indication of a severe exacerbation, likely to be documented fully in the patient's general practitioner records and to be less influenced by subjective perceptions of the effects of new medication. Other objective measures of asthma control are available, but incorporating these into the study would have meant imposing standardisation of treatment upon general practitioners, which is contrary to the safety assessment of marketed medicines guidelines. The pattern of similar hospital admission rates, other unscheduled medical consultations, and adverse event reports indicates that the safety profile of hydrofluoroalkane salbutamol inhaler is similar to that of chlorofluorocarbon salbutamol inhaler.
In randomised clinical trials both the prescriber and patient are often blinded to the medication, but this is clearly not usual in clinical practice. The ability to assess the use of medicines under normal clinical conditions would have been lost had the study been blinded.
The non-interventional design allowed patients who were already using a chlorofluorocarbon salbutamol inhaler to continue this. These patients therefore represented a "survivor population" who were able to tolerate continued treatment, as those unable to tolerate the chlorofluorocarbon salbutamol inhaler would have stopped taking it before the recruitment visit. This factor was identified by the steering committee during the design stage as being likely to result in a higher incidence of adverse events being attributed to the hydrofluoroalkane inhaler because of the change of medication in this group. In interpreting these results, it is the size of this and other related effects--as measured by odds ratios and confidence intervals, rather than just their statistical significance--that is of primary importance. The survivor bias might have been overcome by switching all the patients in the chlorofluorocarbon inhaler group to a single new chlorofluorocarbon salbutamol product. However, this option is not available within the confines of a non-interventional study. Survivor bias is likely to occur in all studies using this design and cannot be eliminated.
The proportion of patients reporting adverse events was similar in both groups, although we confirmed the anticipated phenomenon that more events would be attributed to the new formulation. The events most often considered by general practitioners to be related to the hydrofluoroalkane salbutamol formulation were those commonly associated with salbutamol treatment--headache, nausea, and tremor. This is unlikely to be the result of an increased availability of salbutamol since clinical studies have shown that the adverse event profiles of hydrofluoroalkane inhaler and chlorofluorocarbon salbutamol are the same.[5-8]
The greater attribution of adverse events to the prescription of a new medication was reflected in the higher rate of withdrawals because of adverse events in the hydrofluoroalkane inhaler group. There are a number of reasons for this. Patients are likely to notice a difference in the physical sensation and taste of all reformulated aerosol products, and it is important to educate both doctors and patients during the transition from chlorofluorocarbon propellants to chlorofluorocarbon-free propellants. The lack of educational material in the present study may explain why around 3% patients stopped using the hydrofluoroalkane inhaler because they disliked the taste. The proportion of patients who withdrew fell from 1.9% during the first 30 days to 0.7% in the last 30 days, indicating that with continued treatment patients became used to their new medication. Thus, by the end of follow up, a survivor population for hydrofluoroalkane inhalers was developing in the same way that a survivor population had developed for chlorofluorocarbon inhalers before the study.
Our findings support the experience of clinical trials, showing that the reformulation of salbutamol sulphate in a hydrofluoroalkane propellant system does not result in changes in safety when compared with a chlorofluorocarbon salbutamol formulation. The study design was successful in terms of the number, rate, and geographical spread of patients recruited, and shows that it is possible to fulfil the recommendations of the safety assessment of marketed medicines guidelines. The extent to which postmarketing surveillance studies can ever exclude bias (for example a survivor population) will need further consideration by the safety assessment of marketed medicines' committee.
The authors thank all the general practitioners who contributed patients and data to this study.
Contributors: JGA was chairman of the independent steering committee; CDF, WFH, and DRRW were members of the independent steering committee; JGA and WFH were responsible for clinical input into the design, review and interpretation of data; CDF was responsible for statistical input into the design, review and interpretation of data; DRRW was responsible for epidemiological input into the design, review, and interpretation of data; SMW was responsible for input into the design, review and interpretation of data, as well as for overall study management. JGA will act as guarantor for the paper.
Funding: This study was sponsored by 3M Health Care, Loughborough.
Conflict of interest: SMW is employed by 3M Health Care. The other authors were members of the steering committee, which met under the auspices of 3M Health Care.
[1] Association of the British Pharmaceutical Industry. Guidelines for company-sponsored safety assessment of marketed medicines (SAMM). In: ABPI compendium of data sheets and summaries of product characteristics. London: Datapharm Publications, 1996.
[2] Rawlins MD, Jefferys DB. Study of United Kingdom product licence applications containing new active substances, 1987-9. BMJ 1991;302:223-5.
[3] Waller PC, Wood SM, Langman MJS, Breckenridge AM, Rawlins MD. Review of company postmarketing surveillance studies. BMJ 1992;304:1470-2.
[4] Joint Committee of Association of British Pharmaceutical Industry, British Medical Association, Committee on Safety in Medicines, Royal College of General Practitioners. Guidelines on postmarketing surveillance. BMJ 1988;296:399-400.
[5] Dockhorn R, Vanden Burgt JA, Ekholm BP, Donnell D, Cullen MT Clinical equivalence of a novel non-chlorofluorocarbon-containing salbutamol sulfate metered-dose inhaler and a conventional chlorofluorocarbon inhaler in patients with asthma. J Allergy Clin Immunol 1995;96:50-6.
[6] Kleerup EC, Tashkin DP, Cline AC, Ekholm BP. Cumulative dose-response study of non-CFC propellant HFA 134a salbutamol sulfate metered-dose inhaler in patients with asthma. Chest 1996;109:702-7.
[7] Tinkelman DG, Bleecker ER, Ramsdell J, Ekholm BP, Klinger NM, Colice GL, et al. Proventil HFA and Ventolin have similar safety profiles during regular use. Chest 1998;113:290-6
[8] Bleecker ER, Tinkelman DG, Ramsdell J, Ekholm BP, Klinger NM, Colice GL, et al. Proventil HFA provides bronchodilation comparable to Ventolin over 12 weeks of regular use in asthmatics. Chest 1998;113:283-9.
[9] European Agency for the Evaluation of Medicinal Products. Guideline for post-marketing surveillance studies for metered dose inhalers with new propellants. London: EAEMP, 1995. (CPMP/180/95.) (Accepted 10 August 1998)
RELATED ARTICLE: Key messages
* Credibility of Postmarketing surveillance studies is expected to increase after the introduction of guidelines covering their conduct
* The study design successfully fulfilled the requirements of these guidelines in terms of the number, rate, and geographical spread of patients recruited
* Safety of salbutamol inhalers using hydrofluoroalkane and chlorofluorocarbon as propellants is similar
* Important differences in study design/conduct and outcome between a postmarketing surveillance study and a randomised clinical trial merit further consideration.
Department of Respiratory Medicine, Birmingham Hearfiands Hospital, Birmingham, B9 5SS
J G Ayres, professor
Medical Statistics Unit, London School of Hygiene and Tropical Medicine, London WC 1 7HT
C D Frost, lecturer
Sherrington Park Medical Practice, Nottingham NG5 2EJ
W F Holmes, general practitioner
Division of Public Health, Nuttield Institute for Health, Leeds LS2 9PL D R R Williams, professor
3M Health Care, Loughborough LE1 11EP
S M Ward, clinical research specialist
Correspondence to: Professor Ayres
BMJ 1998;317:926-30
COPYRIGHT 1998 British Medical Association
COPYRIGHT 2000 Gale Group